Policy Brief: COVID-19, A Global Health Concern Requiring Science-Based Solutions
Scientifically-based concrete action points to reduce the spread, lessen the impact, reduce the concerns of the wider population, and avoid further outbreaks for governments, organizations, and individuals are needed
Context
On 31 December 2019, the World Health Organization (WHO) Country Office in China picked up a media statement on the website of the Wuhan Municipal Health Commission on cases of ‘viral pneumonia’ in Wuhan, Hubei Province, People’s Republic of China. The official name of the virus responsible for the outbreak is severe acute respiratory syndrome coronavirus (SARS- CoV-2) according to the International Committee on Taxonomy of Viruses (ICTV), and the disease it causes is named coronavirus disease (COVID-19).
WHO, under the International Health Regulations (IHR 2005), declared the emergence of COVID-19 a Public Health Emergency of International Concern on 30 January 2020 and declared the outbreak a pandemic on 11 March 2020.
WHO detailed a strategic response and preparedness plan1 and produced a Research and Development Blueprint research agenda2 to drive innovation in all aspects of outbreak control, from clinical case management to vaccine development, and developed a master plan for coordinating clinical trials that could lead to potential therapies for patients affected with the COVID-19 disease.
Today, different countries and private laboratories are working to develop effective vaccines using state-of-the-art technology, and simultaneously assessing different treatments, including interferon and other pharmaceutical combinations being used to identify effective therapies. However, we are still trusting of reactive strategies to face this new threat for humanity but working in isolated silos.
What could have been done better to prepare for and reduce the risk of this public health threat? What actions does science suggest for governments, organizations, and individuals in response to this outbreak?
The present contribution of the Health Knowledge-Action Network Steering Committee of Future Health Community (https://futureearth.org/) provides answers based on individual and collective actions, on national and international collaboration, and on multidisciplinary approaches to cope with this pandemic.
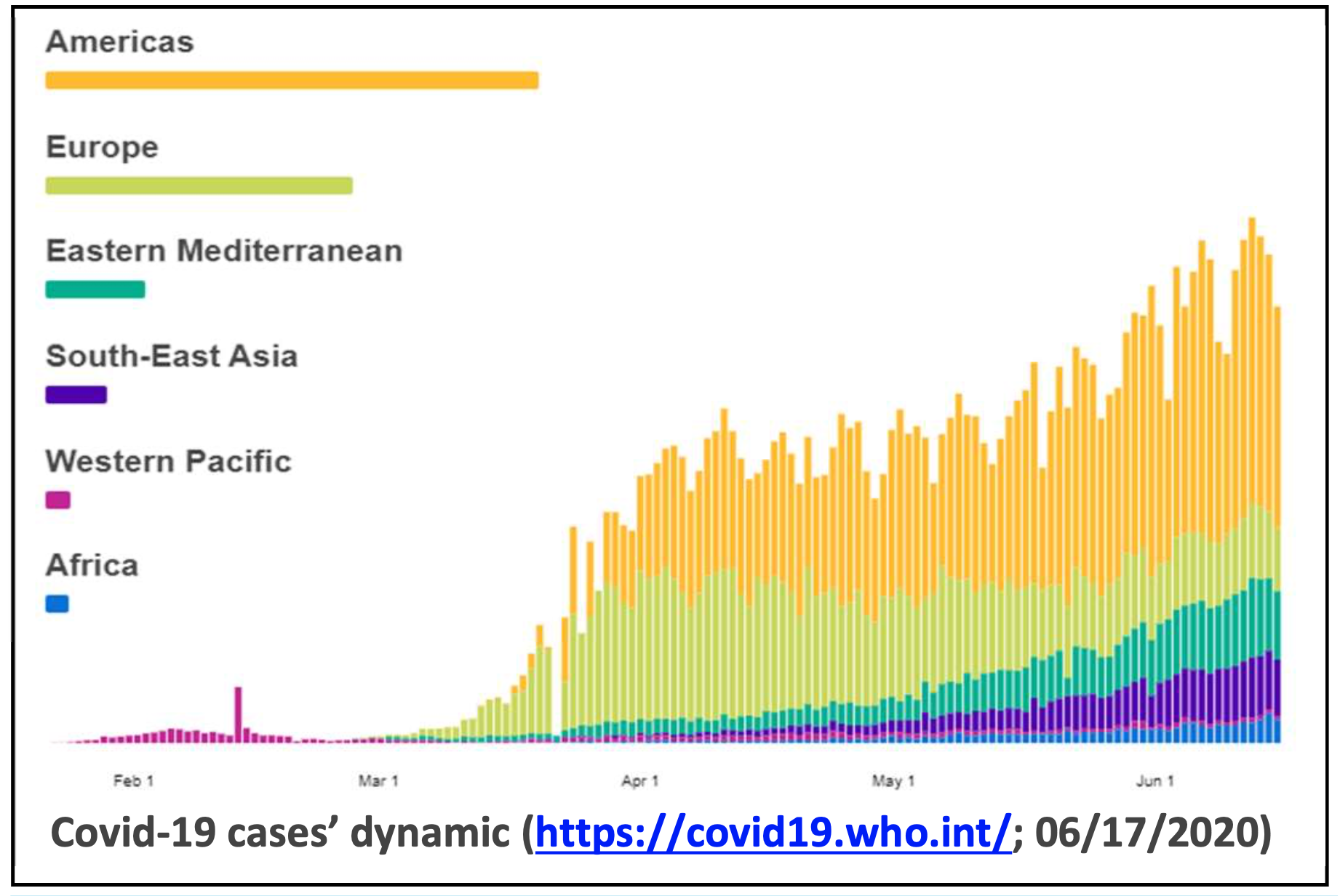
Distribution of the disease worldwide (as of 17 June 20203 – see also the WHO COVID-19 dashboard)
- there were 8,006,427 confirmed cases and 436,899 deaths in more than 200 countries and territories worldwide (mortality rate of 5.5%)
- the majority of confirmed cases were in the WHO Americas region with 3,899,859 cases, followed by Europe region (2,434,184 cases), the Eastern Mediterranean region (796,759 cases), the South-East Asia (486,673 cases) and the Western Pacific region (200,586 cases).
- a broad range of mortality rates are being reported across the countries, territories, and areas with highest rates being reported in Europe, mainly in France (19.2%) followed by Belgium, Italy, UK and Spain with respective rates of 16.1%, 14.5%, 14.1% and 11.1%.
- outbreaks in the WHO African Region evolved moderately the first 3 months since the pandemic reached the region but the number of cases increased rapidly (more than double) in the last 3 weeks. As from 28 March 2020 (10:00 CET), reported cases raised from 2,831 to 83,913 on 26 May 2020 (11:30pm CET) and to 185,070on 17 June (04:00am CET) with a global death rate of 2.3% to date4
Governments’ response challenge worldwide
Since the WHO Public Health Emergency declaration for the COVID-19 outbreak, many countries introduced travel restrictions and other social distancing, non-pharmaceutical interventions, and infection prevention and control measures to try to reduce the spread and the impact of the disease, with profound social and economic consequences.
Fear of exposure is resulting in shortages and massive price-hikes of required personal protective equipment such as surgical masks, despite WHO recommending these, under short supply conditions, only for people with respiratory symptoms or healthcare workers dealing with patients.
Severity among younger age groups of COVID-19 is lower compared to other recent emerging pathogens such as Ebola.
Over 80% of the cases are mild with the severe cases more likely among older adults or people with serious chronic prior illnesses such as heart or lung diseases or diabetes.
Patients that develop pneumonia are at the highest risk.
Symptomatic treatment of respiratory failure places a severe strain on health care systems world-wide, especially to provide intensive care beds and ventilators
What scientists have found
- The epidemic is caused by the SARS-CoV-2 virus, a single strand RNA virus with envelope.
- The main symptoms include mild to severe acute respiratory infection with fever, cough, and difficulty in breathing.
- The primary source of person-to-person transmission is direct exposure through droplets with the potential to seed further outbreaks.
- Coronaviruses (CoV) are zoonotic, which means they are transmitted from animals to humans.
- Close human-wildlife interactions are key to novel viral emergence.
- This is driven by anthropogenic environmental change (e.g. population growth, rapid urbanization, agricultural intensification, illegal hunting and wildlife trade, logging and mining activities that destroy biodiversity and disrupt ecosystems) and increased mobility from previously remote regions – that increase the risk of viruses spilling over and spreading within our globalized population.
- Bats (Fig. 2) are reservoirs of a number of zoonotic viruses5 and although confirmation is needed, a species of Rhinolophus bat is most likely the natural reservoir of the SARS-CoV-2 virus that causes COVID-19.

Action points for Governments
- Adopt a whole-of-government and whole-of-society approach in responding to the COVID-19 pandemic, including involvement of the private sector and civil society organizations.
- Actions taken to address COVID-19 can impact neighbouring countries, the region and beyond.
- For COVID-19 and other emerging diseases that are borderless and have rapidly spread, it is especially important for national governments to coordinate strategies for the collection of data, their analyses, and control and management responses in a manner consistent with the WHO’s technical guidance.
- Work collaboratively and transparently with other countries to support efforts to deal with the COVID-19 outbreak across countries, including quarantine procedures and international transportation, to ensure that cross-border medical and other essential goods supply chains are able to function effectively and efficiently and streamline importation of critical goods and experimental products.
- Ensure free and open reporting of outbreak data and sharing of virus samples, genetic information, and research results to facilitate vaccine and treatment development and ensure equitable and transparent allocation processes for diagnostics, therapeutics and vaccines.
- Develop and implement national research plans and facilitate health care workers and institutions engagement in priority research at regional and global levels.
- Health is central for people’s wellbeing and livelihoods; therefore, governments and other decision makers need to support the health sector in designing and implementing preventative control measures.
- Policies based on scientific evidence are needed to enable the transition to a safe and healthy way of living on this planet, if we are to be prepared for the next virus and to prevent yet another global outbreak.
- There is a need for increased investment in capacity building for public health in low-and middle-income countries and building resilient health systems that can detect, prevent, respond, and quickly recover from outbreaks and other health emergencies.
- National governments should shift their operational stage from regulating points of entry to reflect the situation in countries.
- Where more infection is spreading widely within the community, that calls for social distancing as a preventive strategy and an urgent scale-up of aggressive measures to combat COVID-19.
For prevention and response measures within countries:
- WHO recommends to test every suspected COVID19 case.
- If positive, then isolate them and trace their close contacts within up to two days before symptoms developed and test those people too.
- Focus on prompt diagnosis and provide optimal care of cases and take a holistic approach to the health care system to maintain system functioning for the treatment of other diseases.
- The health care system should remain fully operational while responding to the serious cases of COVID-19.
- Develop guidelines and protocols based on sound scientific advice to 1) respond to the serious cases; 2) reduce further spread in society and among healthcare workers; and 3) increase early case detection and reporting to avoid overloading hospitals.
- Where possible, 1) maintain societal activities, including business activities that are important for health care systems to continue to function: 2) create and maintain community support channels / groups, support required for mental health and wellbeing and the right environment for community support to health care providers (for instance, providing safe, secure living conditions; looking after their home based needs such as children and elderly at home, and so on, as front line care providers work for long hours); 3) contain geographical spread from densely populated spaces to less populated ones and from urban to rural areas.
- Halt sharing of misinformation and discriminatory posts, international or not, especially on social media, through public education and outreach activities, because false information can disrupt response efforts at managing the epidemic.
- Provide evidence-based information to organizations and individuals through health agencies and professional associations on websites, news outlets, and through local governments to explain the situation and to prevent potential spread within new communities.
- Provide an emergency call center number for people with questions about their symptoms, what precautions they can take, and what protocol they should follow.
Action points for organizations
- We call on scientific, governmental and non-governmental organizations in the field of conservation, ecology, epidemiology, public health, mathematics and computer science, governance, planning, geography, the science of cities, sustainability science, and many others to work collaboratively to prevent future outbreaks and other health risks and disasters to people and the planet, by applying a systems-based approach (EcoHealth, OneHealth, Planetary Health and Urban Health communities).
- Research organizations can improve understanding of the causes, risks, infectiousness, severity and threats of a pandemic in communities.
- Health organizations can emphasize the importance of human behavior in disease emergence, and what can be done to avert the emergence and spread of these diseases.
- Conservation organizations can communicate openly about the fact that wildlife commonly carry pathogens that can be lethal to people and to increase awareness that the risks of pathogens affecting human health often results from unsustainable transformations of our natural environments and ecosystems that provide life-supporting services for our health.
- Reassure the public that ownership of pets, livestock, and presence of wildlife in a community is not necessarily a public health risk, and that the key issue in an outbreak or a pandemic is transmission from person to person through contact with infected people.
- Emphasize infection prevention and control measures, especially when caring for the sick.
Within an organization, actions to protect your employees and your business include:
- Work collaboratively to provide information for employees and customers to avoid spreading the disease and its associated health impacts.
- Provide facilities for hand sanitation with soap and water, alcohol-based hand rub, or antiseptic hand wash and display posters promoting handwashing.
- Ensure workplaces are clean and hygienic and disinfect surfaces regularly.
- Advise employees to stay at home even if they just have mild symptoms of COVID-19.
- Adjust operations to avoid direct close contact among people to prevent spread when an organization or branch office is located in a high-risk zone.
- If there is an episode of infection in your organization, then contact your government immediately and follow containment measures.
- Consult national travel advice before organizing business trips.
- Develop and use information and educational materials to address fears and attitudes within your organization.
- This will help focus efforts to prevent disruption from disinformation especially via social networks.
- Develop strategies and contingency plans (including digital solutions, distance work, logistics, insurance) to improve preparedness for future epidemics and other disasters.
Action points for individuals
- Individuals can protect themselves from infection and also support government and organizational efforts to deal with the pandemic.
- Individuals should wash their hands frequently, avoid touching their mouth, eyes, and nose too often, avoid dense crowds of people, maintain social distances of at least 1 meter (3 feet) from others who are coughing or sneezing or have other respiratory symptoms, have suspected COVID-19 infection with mild symptoms, or are caring for someone with suspected COVID-19 infection, and avoid staying in poor ventilation areas with those persons.
- Follow good respiratory hygiene practices by covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. Then dispose of the used tissue immediately.
- Wearing a mask is necessary in public settings with poor social distancing and if you have symptom of a respiratory infection – this will help slow community-based transmission of the virus.
- Stay home if you feel unwell and seek medical care promptly if you experience fever, cough, and difficulty in breathing as this may be due to a respiratory infection or other serious condition; use a telephone or other means of remote access (e.g. apps) when available.
- As a general precaution, practice good hygiene when visiting live animal markets, wet markets, or animal product markets, and avoid consumption of raw or undercooked animal products.
- Follow reputable sources of information to stay up to date on the developments and suggestions through your national and local public health authorities.
- Continue your daily operations – with the additional points above unless requested otherwise by your local government or organization, or if you are based in a high-risk zone with known cases.
- Follow advice given by your healthcare provider.
- Take corrective action on any discriminatory posts and wrong information occurring in social media to prevent delays in responding to the outbreak by reporting to local or national authorities and avoiding sharing
References and additional suggested reading
1https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdf
2https://news.un.org/en/story/2020/02/1057161
3WHO dashboard on coronavirus https://covid19.who.int/
4https://www.afro.who.int/health-topics/coronavirus-covid-19
5Hu B, Zeng LP, Yang XL, et al. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog. 2017;13(11):e1006698. Published 2017 Nov 30. doi:10.1371/journal.ppat.1006698
6G. B. Sioen, P. Daszak, K. Ebi, C. Wannous, B. Kone, K. Bowen, F. W. Gatzweiler, F. Harris, M. Boeckmann, A. Morse, C. Watanabe, J. J. K. Jaakkola, G. O Dida, W. Ma (submitted) Emerging viruses are a global health concern requiring science-based solutions and local action.Journal of Global Change Data & Discovery
Authors and Affiliations
Health Knowledge-Action Network Steering Committee Members;
Authors have contributed equally to drafting and finalizing the brief
Contact: health@futureearth.org
The Future Earth Health Knowledge-Action Network was formed in 2016 and consists of 227 global members with the vision to support and enable solution-driven transdisciplinary research and action to improve understanding of how global and regional environmental changes can affect population health and health systems.
The Health Knowledge-Action Network Steering Committee is comprised of individuals with international standing on global environmental change and public health
Download the PDF:
DATE
June 26, 2020AUTHOR
Future Earth Staff MemberSHARE WITH YOUR NETWORK
RELATED POSTS
COP28: Health is Finally on the Agenda – But There’s More to do as We Face Continued Climate Extremes
International Day of Clean Air for Blue Skies
Future Earth Providing More Funding for LMIC Participation in Belmont Forum Call